July 11, 2023 – Kathy Blackwell is not going to allow a couple of aching joints stop her from living her best life.
The 73-year-old resident of Simi Valley, a bedroom community about 30 miles northwest of downtown Los Angeles, organizes regular activities for her group of seniors. The 20- to 30-member-strong band of seasoned citizens, mostly women, keep active. Over the coming weeks, they plan to catch the Beach Boys at the historic Hollywood Bowl and take a cruise to Alaska.
The busy schedule is why Blackwell intends to delay her second hip replacement surgery, opting instead for a cortisone shot in hopes of easing the pain enough to enjoy the upcoming excursions.
Not that she is shy about joint replacement. If her orthopedic surgeon offered a frequent customer punch card like the ones you get at the local coffee shop, hers would be nearly full. Blackwell’s knees and a hip have been replaced, and her other hip will be, too, once her calendar clears up.
“If you go on enough with chronic pain where there’s no relief, you get cranky,” Blackwell said.
More Than 1 Million New Knees, Hips
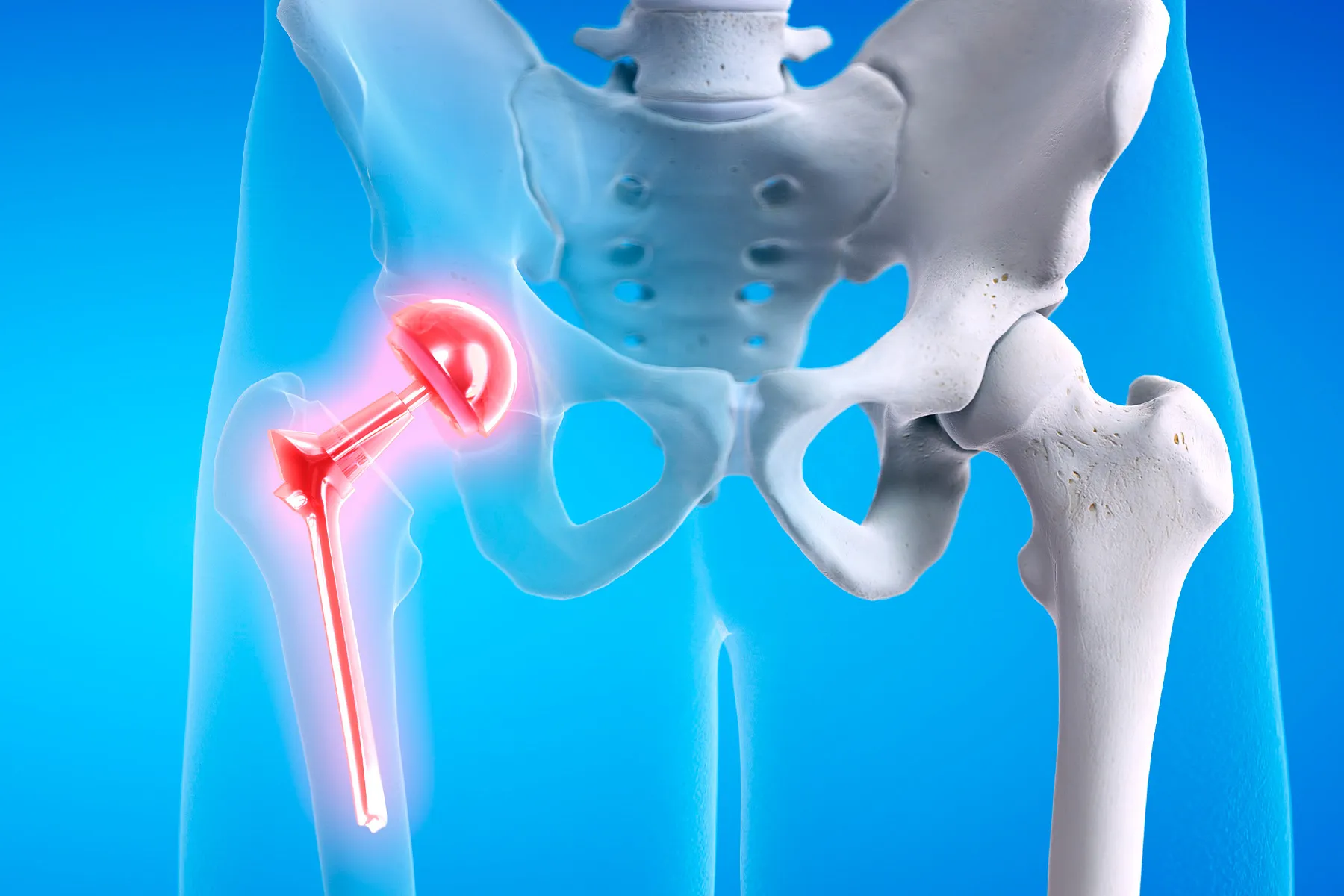
Joint replacements are getting more common, with about 790,000 total knee replacements and more than 450,000 hip replacements performed annually in the United States, according to the American College of Rheumatology.
Experts agree age is not a factor when considering candidates for joint replacement. Rafael Sierra, MD, of the Mayo Clinic, said he’s done hip replacements on patients as young as 12 and as old as 102. Orthopedic surgeon John Wang, MD, of the Hospital for Special Surgery, in New York City, has performed a total knee arthroscopy on a patient in their mid-90s. At 73, Blackwell is on the older side of the average age of 66 for a hip replacement.
“A lot of research and studies have shown that no matter what the age ranges, people end up doing great,” Wang said.
More importantly than age, older patients should be prepared for post-surgery therapy and treatment. For younger patients, the biggest drawback is outliving the estimated 25-year life span of a joint replacement. Complications are rare and occur in about 2% of procedures. These include infection, dislocation of the joint, and blood clots; other health issues you also have are not a factor.
Considering Blackwell’s hard time with her first knee replacement, it’s no small wonder that she ever set foot in a surgeon’s office again.
After putting it off for 7 years, Blackwell finally agreed to her doctor’s advice to replace her left knee in 2017 to relieve what she described as a “grinding,” chronic, bone-on-bone pain.
“It got to the point where there were no alternatives,” she said.
But her first orthopedic surgeon did a “lousy job,” leaving her with a gaping, festering wound that resulted in sepsis and required wound vacuum therapy to close the lesion. She eventually found another surgeon who removed and cleaned up her artificial knee before replacing the prosthesis. Luckily, the sepsis didn’t spread, and eight surgeries later, she was in the clear.
Blackwell’s second knee replacement in 2018 was a textbook surgery, as was a hip replacement in late 2019 .
“Your whole attitude changes,” she said.
What Generalists Should Know
Orthopedic surgeons recommend that primary care doctors ask two things when weighing joint replacements: Have they exhausted nonsurgical treatments, and is the pain intolerable? They also advise avoiding narcotics to treat the symptoms.
The top issue to consider for a primary care doctor when weighing whether their patient may be a candidate for joint replacement is if the pain and the imaging are bad enough to warrant surgery.
“You don’t want to do it too soon,” Sierra said.
Sierra likes to tell the story of the golfer whose knee stiffens after playing 18 holes. To those patients, he recommends dialing back the activity; in this case, using a cart or playing only nine holes.
Wang agrees, asking if the pain is “lifestyle-altering” and if the patient was unresponsive to nonsurgical treatments such as over-the-counter medications, anti-inflammatory meds and shots, home exercises or physical therapy, wearing a brace or sleeve, or simply changing their activity.
And no addictive pain pills to treat arthritis that can lead to other serious issues.
“This is not going to heal itself,” Wang said. “It’s not going to improve on its own. So, we don’t want to throw narcotics at it just to cover it up.”
Karen Smith, MD, has been a family doctor in rural North Carolina for more than 30 years. When she sees patients complaining about their joints, she first looks at function and pain. From there, she explores why they’re having discomfort. For example, is the problem an ergonomic issue at work or the result of carrying a lot of body weight?
“We look at those areas to determine what can be modified,” she said. “All of that’s done even before we get to having the orthopedic involvement.”
Smith said she also considers things beyond basic medicine: What is the patient’s mental status and tolerance for pain? Do they have a support system at home for post-operative care? And can they afford to miss work?
“We look at all of those factors together because that is going to determine the outcome that we’re hoping to achieve,” Smith said.
Great Expectations
A recent study shows that older patients respond better to knee replacements than younger patients, particularly with pain relief and quality of life. The reason for this is believed to boil down to expectations. Whereas a younger person may want to return to the racquetball court and perform like they used to, older patients may just wish to walk down the hall without discomfort.
“It’s possible that these under 55-age-old patients may just take a little longer to heal to be satisfied,” Wang said. “We really can’t speak to why this is happening, but it’s possible that the younger patients are more active, and they expect more out of their knee.”
Jeevan Sall, MD, is a primary care sports medicine doctor with Providence Mission Heritage Medical Group in Laguna Niguel, CA. He first discusses conservative management for patients struggling with arthritis in their joints. These measures include rehabilitation exercises, braces, shoe inserts, medication, and weight loss efforts. If these steps don’t improve a patient’s pain or lifestyle, surgery is on the table. Managing expectations is a significant factor.
“Is the patient mentally ready for surgery?” Sall said. “This includes what they hope to achieve with surgery as well as the risk and benefits of the procedure.”
Blackwell’s hip and knee pain came simply from a life well-lived, with no marathon running or life-changing accident to speak of. She worked as a housewife raising her two children and owned an elevator company with her late husband, Robert Blackwell.
Yes, the elevator construction business has jokes.
“We have our ups and downs,” Blackwell said.
And with her new joints, so does Kathy.
24World Media does not take any responsibility of the information you see on this page. The content this page contains is from independent third-party content provider. If you have any concerns regarding the content, please free to write us here: contact@24worldmedia.com